Measles Outbreaks In US Unfolding In A Familiar Epidemiologic
Pattern
CDC Testimony
Calls Situation A Wake-Up Call About US Vaccination Challenges
A total of 228 cases of measles have been reported as
of mid-March in the United States and these have garnered headlines
across the country with regular updates on the nightly news. Many of
these reports have been focused on people opposed to vaccine school
laws or hesitant to have their children vaccinated. This latter
“vaccine hesitancy” behavior has been identified by the World Health
Organization as one of ten threats that will require global attention
in 2019.
The Outbreaks
To date, measles has been reported from 12 states and 6
of these jurisdictions have
been labeled as
outbreaks because they have 3 or
more cases (New York, Rockland County, New York City, Washington,
Texas, Illinois, and California.)
Most of the publicity about the cases in 2019 revolves
around the outbreak in Washington state which has reported 72 cases,
all but one of them in Clark County Washington, and all but a handful
of these among unvaccinated persons 18 years or younger.
Clark County has been known to be at risk for this kind
of outbreak because approximately 25% of kindergarten children in the
2017-18 school year did not have all their recommended doses of
vaccine and that number was as high as 40% in three schools, according
to Washington State health data. This high degree of susceptibility
provided fertile territory in which to start a measles outbreak.
According to Scott Lindquist, a state epidemiologist quoted in
media accounts, the outbreak for the first 70 cases has cost the state
well over $1,000,000 or over $14,000 per case so far.
Epi Situation
Given the intense level of national news coverage, it
is easy for the casual observer to get the impression that these cases
represent an unusual situation in the US. In reality, it is the
contrary.
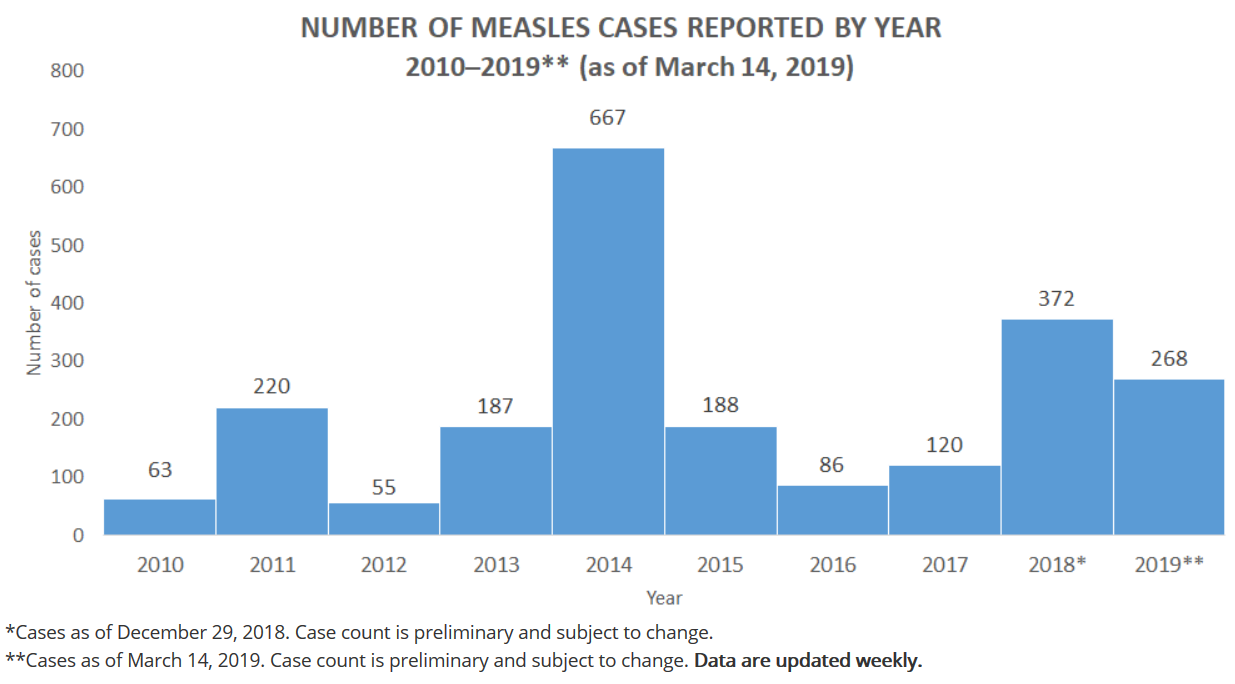
Why? The number of
cases each year since 2000 when measles was declared eliminated from
the US has ranged from a low of 37 to a high of 667 and the 2019 cases
are in that range so far.
The number of cases in
2019 so far is actually striking evidence of the efficacy of the
measles vaccine program since prior to widespread use of the vaccine
there were 3-4 million cases per year, 400-500 deaths and numerous
complications. Measles vaccination coverage is reported to be 92%,
another indication of the high level of protection in the overall
population.
So What’s The Problem?
What drives measles
epidemiology each year in the US is 1) the number of travelers who get
measles while abroad and bring it back to the US, and 2) the number
and size of the pockets of unvaccinated persons waiting for them at
home making it possible for the virus to spread domestically,
particularly within the vulnerable subgroup.
Why Pockets of
Susceptibles
Subgroups of
susceptibles exist because of a variety of reasons. Looking back over
the outbreaks in recent years indicates that cases have occurred in
Orthodox Jewish communities, a Somali-American community with poor
coverage, Amish communities, and now the latest in Clark county
Washington.
These subgroups often
exist because all but three states allow exemptions from vaccination
for religious or philosophical reasons and these exemptors often
cluster together geographically. Also, because of health disparities,
clusters of people who lack health insurance, are poor, or live in
rural areas may be at increased risk.
Also, the number of
imports as opposed to outbreaks each year depends on the incidence of
measles in other parts of the world which rises and falls and on the
number of susceptible American travelers who visit these countries.
Vaccine Hesitancy
According to Nancy
Messonnier, Director of CDC’s National Center for Immunization and
Respiratory Diseases who testified at a recent congressional hearing,
“vaccine preventable diseases do not have the visibility they once had
and many parents question whether the vaccines are more dangerous for
their child than the disease they prevent. Parents also have access to
conflicting and often inaccurate information about vaccines via the
Internet, and others express concern that there are too many vaccines.
Before 1985, the recommended immunization schedule included seven
vaccines. Today we can protect children younger than 2 years of age
from 14 potentially-serious diseases with vaccines.”
These are among the
causes of non-vaccination usually lumped under the “vaccine hesitancy”
threat highlighted by WHO.
Other Challenges
In describing the
overall state of the US vaccination program, Messionnier pointed out
other important challenges where disease prevention is sub-optimal.
For example, influenza vaccination coverage for children is typically
less than 60% and this coverage varies by state. Over the last four
influenza seasons influenza has killed almost 500 children. Some of
the same barriers to immunization are at work for this vaccine
According to
Messonnier, only 50% of adolescents in the US are receiving all
recommended doses of human papilloma virus (HPV) vaccine to get
protected against cancers caused by HPV.
Wake Up Call
Messonnier told
congressmen that the increase in measles cases and the current vaccine
situation should be seen as a wake-up call that more needs to be done
to maintain and even increase the enormous health and societal
benefits of associated with optimal use of recommended vaccines.
Chart below is from
the Centers for Disease Control and Prevention.
https://bit.ly/2iMFK71
|