|
Excess Deaths Provide Additional Estimate Of The
Burden Of Disease Related To
COVID-19
Absence Of Excess Deaths Might Also Be Used As An Indicator That
Community Risk Level Has Returned To “Normal”
The
Centers for Disease Control and Prevention (CDC) is providing
provisional counts of weekly deaths from all causes to supplement
routinely reported counts of deaths due to COVID-19. When compared to
the expected number of deaths from all causes over recent years, the
number of excess deaths can provide another measurement of the overall
impact of COVID-19. This is useful since COVID-19 related mortality
may be undercounted in the routine reporting.
Incomplete Count
And that
is precisely what an investigation of these deaths is showing. As
reported in an ongoing NY Times analysis of the CDC data, an estimated
211,500 more
people have died than usual in the US from March 15 to Aug. 1 2020.
This analysis adjusts current death records to account for typical
reporting lags. The number of deaths from all causes is 56,000 more
than the official count of coronavirus deaths for that period.
Even later as of mid-August, the official CDC death count from
COVID-19 is 171,012, well below the 211,500 figure.
In
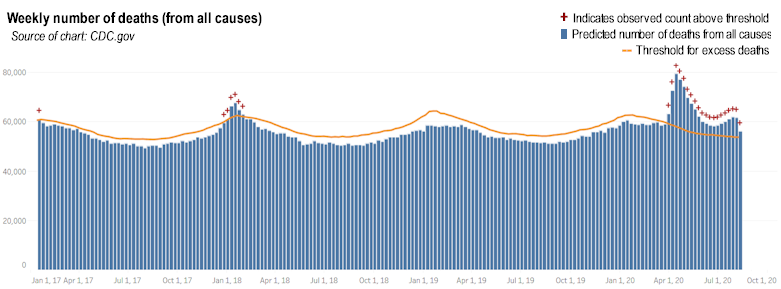
looking at the actual number of weekly deaths from all causes in the
United States in 2017-2019 before the pandemic, the number of weekly
deaths varies by season but the number and pattern is relatively
consistent from year to year. For example, during the period
April-June of 2019, the number of weekly deaths ranged narrowly from a
low of approximately 52,000 to 57,000. In 2020 that weekly number has
ranged more broadly from a low of approximately 59,000 to a high of
approximately 79,000 in the spring. Stated differently, the percentage
increase of deaths over the threshold (defined as the average expected
number of weekly deaths in 2020)
ranged from a low of approximately
10% to approximately 40% higher
than normal.
| |
|
|
| |
 |
|
| |
|
|
The estimated number
of deaths from all causes may contain deaths from COVID-19 that were
not diagnosed because of lack of testing or misclassified for other
reasons. Also, the deaths from all causes would include deaths brought
about indirectly by the pandemic virus because of health care
shortages, overwhelmed health care systems, or even suicides. The
average number of deaths used for comparison in calculating the excess
number of deaths does not take into consideration any changes that
could have lowered the expected number of deaths because of behavior
changes such as lowered risk from less automobile driving.
Excess Deaths As
Indicators
Much discussion during
the pandemic has centered on what indicators might be used to decide
that it is safe to open schools or safe for persons to resume their
normal lives by eating in restaurants or going to the gym. Some
suggested indicators have been the reported number of cases, the
percentage of persons testing positive for SARS-CoV-2, the testing and
contact tracing capacity, or the number of hospitalizations for COVID.
Each of these has its shortcomings that are difficult to quantify but
which affect the reliability of the number as a valid indicator of
personal or community risk. Deaths are definitive and the count is
considered relatively complete and so it has perhaps greater
reliability as an indicator of the risk of acquiring COVID. When the
number of excess deaths falls below the threshold expected, this might
be the time to declare an all-clear for the community and resume
normal activities.
Threat Level Schemes
Some health officials such as those in
Harris County Texas have attempted to measure community risk levels by
publishing a color coded scheme for each level of risk. These levels
are #1 Severe Uncontrolled Community Transmission, #2 Significant
Uncontrolled Community Transmission, #3 Moderate Controlled
Transmission, and #4 Minimal Controlled Transmission. Among the
criteria used to establish the different threat levels, there is no
mention of excess deaths. The lowest level of risk achievable is
described as “minimal controlled transmission”. Such a minimal risk
level may still be unacceptably high for vulnerable individuals 65 or
older or persons with pre-existing conditions since even in this
scheme persons are advised to leave home only as necessary. These
individuals could resume normal lives more safely and more confidently
if SARS-CoV-2 circulation was low enough not to be causing any
measurable increase in the expected number of deaths. This is
potentially important because even with an effective vaccine,
SARS-CoV-2 may become an endemic virus and a total halt of viral
circulation may not be achievable. The other more frequently used
measures of viral activity could also be factored in.
■
|