|
COVID Monthly Recap
By invited
columnist Katelyn Jetelina, MPH PhD, aka, Your Local Epidemiologist
[Editor’s Note:
We have been following the blog posts created by University of
Texas Health Science Center epidemiologist Katelyn Jetelina during the
COVID pandemic. Calling herself Your Local Epidemiologist, Katelyn has
garnered hundreds of thousands of followers among both lay and
professional readers for her science-based yet timely, clear and easy
to understand descriptions and visualizations of the latest findings
and recommendations about COVID-19. Given the pace of new developments
over the last 19 months, and the regular frequency of her posts, this
is no small accomplishment. She has become internationally recognized
for her skillful communication of the science around COVID with her
newsletter reaching 27 countries and actively translated into 6
languages. The Epidemiology Monitor has invited Dr Jetelina to recap
the key developments she reports on each month, beginning in this
month with a recap of the main findings from September. Please look
for these summary reports over the coming months as COVID developments
continue to unfold. Let us know your thoughts about these
recaps. Send comments to
mailto:editor@epimonitor.net]
COVID-19: September
Summary
State of Affairs
Thankfully, in
mid-September, the United States’ Delta wave peaked and the national
average of cases decreased 30% by the end of the month. In September
we also saw the dominant hot spot migrate: It moved from the South to
the mid-Atlantic (South Carolina, Tennessee, and Kentucky) and ended
September in in Alaska.
And, although severe
indicators lag, we’ve seen hospitalizations and deaths make their
descent too. As of September 30, there were 83,224 people hospitalized
with COVID compared to103,006 hospital admissions at Delta’s peak. By
the end of September, we were averaging 1,927 deaths per day due to
COVID19 (Delta’s peak was 2,087).
Severe cases, at this
point of the pandemic, are largely preventable. But, regardless, in
September COVID-19 was the
leading
cause of death in the United States. According to the Kaiser Family
Foundation, 49,800 deaths in September would have been prevented with
vaccines.
We are hopeful,
though, that case, hospitalization, and death trends will continue to
decrease. Interestingly, Delta waves across the globe had a distinct
pattern: 2.5 month flare of virus until retreat. So why doesn’t the
virus just spread and spread until it has no more people to infect?
It’s a simple, legitimate question with a very complicated answer: We
don’t know. There’s no scientific consensus on why this happens. We
hypothesize it’s largely driven by the combination of
four
factors: 1) human behavior; 2) social networks; 3) seasonality; and 4)
level of vaccination/natural immunity. There has been much discussion
whether this is the last wave of the COVID19 pandemic. At this point
it’s certainly partially (if not fully) dependent on the durability of
natural immunity.
Vaccines
There was one silver
lining to the Delta wave, though: vaccination rates increased. This
uptick was due to Delta, hospitals filling up, knowing someone who got
seriously ill or died, or wanting to participate in activities (like a
concert). We continue to live in a reactive (rather than proactive)
society.
At the end of
September,
55% of
Americans were fully vaccinated (64% with at least one dose). 65% of
the eligible population (12+ years) was fully vaccinated. This
vaccination rate ranked the United States as #48 in the world despite
leading the science, manufacturing the vaccines, and having plenty of
supply.
September was also the
start of a contentious debate about boosters. Many scientists argued
that we don’t need boosters because we haven’t seen waning protection
in hospitalizations and deaths in the United States. On the other
side, scientists argued that we shouldn’t have to wait if we’re seeing
robust evidence of waning immunity in Israel (the first country to
vaccinate a majority of their population).
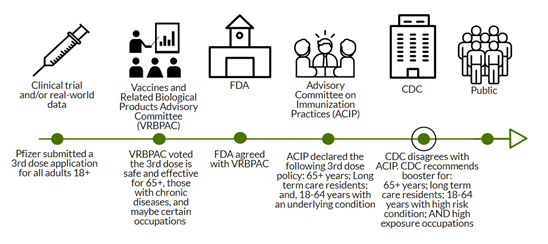
This debate was put
under the spotlight on September 17 when the external scientific
committee to the FDA (called VRBPAC) met to discuss Pfizer’s
application for a booster. After reviewing the data and voicing
frustration with the lack of data in the United States, VRBPAC
ultimately decided that a Pfizer booster was safe and effective. The
committee
recommended that those
65+, those with chronic diseases, and those with certain occupations
should get a a booster. The FDA agreed with its advisory board.
Then the ball was
punted to ACIP (the external scientific advisory committee to the
CDC). Because these boosters are under Emergency Use Authorization and
funded by the government, the CDC has ultimate policy decision making
power. After 2 days of deliberations, ACIP decided that only 65+ and
18+ with chronic diseases should get a booster. The next day, CDC
modified the advice of their external advisory committee and also
approved the booster for high exposure occupations. This is a highly
unusual move, but it aligned FDA and CDC recommendations for a Pfizer
booster.
Variants
Also, in September, a
new variant came onto our radar: Mu. On August 31, the WHO
announced
this new SARS-CoV-2 variant as a “Variant of Interest”.
Briefly, Mu was first
discovered in Colombia in January 2021. It since spread across the
globe, including the United States. There was considerable interest in
this variant because, as the WHO stated,
it has a “constellation of mutations that indicate potential
properties of immune escape”. In other words, there are number of
changes on the virus in which our treatments and vaccines may not
recognize, and, thus not work.
In September, the WHO announced it
was closely watching how Mu competed with Delta in Colombia and
Ecuador. Can Mu outcompete (i.e. more transmissible) Delta?
Because if it can, we may be in trouble.
What to look for in
October?
We hope to watch
trends continue to decrease and hope to watch Mu not overtake Delta.
October will be a big vaccine month, as we will get a lot of questions
answered about boosters for other vaccines and, finally, will the FDA
and CDC recommend a vaccine for 5-11 year olds?
Stay tuned. ■
|